Using human skin to cure the world’s deadliest brain cancer
The answer: This development had a 25:1 failure ratio in clinical trials over the course of 16 years, between 1998-2014. (The question to this answer will be revealed at the end of this article: no cheating!)
“Everyone should know this stuff” Level
Glioblastomas are a type of brain tumor which are typically very malignant. They reproduce quickly because a solid network of blood vessels nourishes them. Brain cancer is one of the deadliest cancers; it is one of just eight types of cancer whose projected three-year survival rate is below 50% (“Cancer Facts & Figures 2014,” 2014). Of malignant brain cancers, glioblastoma is the most common and most lethal among adults (“Tumor Types: Understanding Brain Tumors,” 2016).
Effective and fast treatment is important in order to combat the rapid-spreading tumor and relieve patients of damaging, painful symptoms, and to aid or even save the lives of many; over 10,000 new cases of glioblastoma arise every year (Bagó et al. 2017).
Treatment approaches vary due to the variety of cells that may make up glioblastomas. Most involve surgery followed by chemotherapy and radiation therapy (“Glioblastoma (GBM),” 2014). It is impossible for doctors to surgically remove a glioblastoma completely because of its ability to rapidly and sporadically branch into healthy brain tissue. Surgery can be dangerous around parts of the tumor that extend into vital regions of the brain, such as speech and coordination (“Tumor Types: Understanding Brain Tumors,” 2016).
A team from UNC-Chapel Hill led by Shawn Hingtgen conducted a study which may be the answer to effective treatment of glioblastoma. Scientists are already aware of and have tested the ability of neural stem cells, or stem cells in the brain, to track down brain cancer; however, harvesting these cells from the patient’s brain can be difficult because it requires invasive surgery (Hiolski, 2017).
Hingtgen came up with a technique called “skin flipping;” he and his team created neural stem cells out of a patient’s own skin cells (“Revolutionary approach for treating glioblastoma works with human cells,” 2017). One major benefit of this treatment is that the cells come from the patient’s own body, and therefore will not cause an adverse immune reaction. One of the researchers on the team, Matthew Ewend, M.D., said, “It doesn’t require immunosuppressant. It’ s not a foreign tissue, and so there’s no chance of rejection of the tissue. Everybody has a source for this, so every patient could be a candidate” (Bennett, 2017).
Another key asset to this technology is the speed with which the cell can be transformed. Said Hingtgen, “It used to take weeks to convert human skin cells to stem cells. But brain cancer patients don’t have weeks and months to wait for us to generate these therapies. The new process we developed to create these stem cells is fast enough and simple enough to be used to treat a patient” (Bennett, 2017).
The team’s next task was to engineer the stem cells to carry therapeutic agents which kill the cancer. The stem cells create a small “halo” of a drug around themselves, and then kill the cancer cells by bumping against them. Thus, they avoid exposing other parts of the body and brain to damage (Bennett, 2017).
“For geniuses only” Level
One of the major and unique advantages of Hingtgen and his team’s method is the fact that the induced neural stem cells (iNSCs) are autologous. This is beneficial not only because it eradicates the risk of immune rejection, but also because it addresses certain problems allogeneic therapies face. The iNSCs provide a longer window of drug administration due to reduced immune response, which allows for increased cancer cell death and tumor suppression. Compared to allogeneic therapies which activated leukocytes and microglia, immune system cells, Hingtgen’s team’s autologous therapy found greater amounts of self-derived induced pluripotent stem cells (iPSCs) which caused minimal immune activation. Therefore, this team’s engineered, therapeutic iNSCs may have the potential to be more effective treatment than other allogeneic treatment methods.
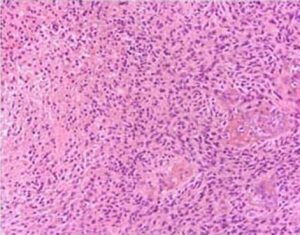
Close up of glioblastoma cells (Bruce, 2016)
Impress your friends and family with these three related facts:
Fact 1: Cancer of the brain and central nervous system is one of the most common cancers among children aged 0-14, at 16% (“Cancer Facts and Figures 2014,” 2014).
Fact 2: In Hingtgen’s study, stem cells were used to treat and kill cancer. Scientists have also researched a completely different type of stem cell, cancer stem cells, which make up about 1- 3% of a tumor, and are targeted as the source of the cancer’s growth (“Cancer Stem Cell Research Frequently Asked Questions (FAQ),” 2016).
Fact 3: Scientists have been able to associate around 80% of cancers with metastasis to the brain. Nearly 50% of melanoma cases metastasize to the brain (“Quick Brain Tumor Facts,” 2014).
The question: What is the success rate of developing brain tumor treatments (“Quick Brain Tumor Facts,” 2014)?
About the author: This page was created by Grace Zhang, a freshman at Choate Rosemary Hall in Wallingford, CT. Grace’s spirit animal is the whale. Someday, Grace will be famous for being the first student to start an independent whale sanctuary.
Works Cited
Bagó, J. R., Okolie, O., Dumitru, R., Ewend, M. G., Parker, J. S., Vander Werff, R., . . . Hingtgen, S. D. (2017). Tumor-homing cytotoxic human induced neural stem cells for cancer therapy [PDF]. Science Translational Medicine, 1-13. Retrieved from http://stm.sciencemag.org/
Bennett, A. (2017, February 2). ‘A big step’: UNC researchers use stem cells to treat brain cancer. Retrieved February 5, 2017, from News Observer website: http://www.newsobserver.com/news/local/education/article130353414.html
Brain Tumor Statistics. (2014). Retrieved February 14, 2017, from American Brain Tumor Association website: http://www.abta.org/about-us/news/brain-tumor-statistics/
Bruce, J. M., M.D., & Kennedy, B., M.D. (2016, December 13). Glioblastoma Multiforme (H. H. Engelhard, III, M.D., Ph.D, FACS, Ed.). Retrieved February 14, 2017, from MedScape website: http://emedicine.medscape.com/article/283252-overview
Cancer Facts & Figures 2014. (2014). In American Cancer Society (pp. 1-70). Retrieved February 14, 2017, from https://www.cancer.org/content/dam/cancer- org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2014/cancer-
Cancer Stem Cell Research Frequently Asked Questions (FAQ). (2016, March). Retrieved February 15, 2017, from Michigan Medicine website: http://www.mcancer.org/research/stem-cells/faq
Glioblastoma (GBM). (2014). Retrieved February 14, 2017, from American Brain Tumor Association website: http://www.abta.org/brain-tumor-information/types-of-tumors/glioblastoma.html?referrer=https://www.google.com/?referrer=http://www.abta.o rg/brain-tumor-information/types-of-tumors/glioblastoma.html
Hiolski, E. (2017, February 1). Reprogrammed skin cells shrink brain tumors in mice. Retrieved February 5, 2017, from ScienceMag website:
http://www.sciencemag.org/news/2017/02/reprogrammed-skin-cells-shrink-brain-tumors-mice
Quick Brain Tumor Facts. (2014). Retrieved February 15, 2017, from National Brain Tumor Society website: http://braintumor.org/brain-tumor-information/brain-tumor-facts/
Revolutionary approach for treating glioblastoma works with human cells. (2017, February 1). Retrieved February 5, 2017, from ScienceDaily website: https://www.sciencedaily.com/releases/2017/02/170201162507.htm
Tumor Types: Understanding Brain Tumors. (2016). Retrieved February 14, 2017, from National Brain Tumor Society website: http://braintumor.org/brain-tumor-information/understanding-brain-tumors/tumor-types/#glioblastoma-multiforme

Leave a Reply